Breast cancer screenings, self-exams, and the impact of genetics.
While breast cancer is symptomatic for some, for many, breast cancer occurs with few warning signs and this can be very detrimental. When found at later stages, breast cancer often requires more rigorous treatments. To prevent late detection, the American Cancer Society recommends that women begin yearly breast screenings at age 45. Breast screening can include mammograms, thermography, ultrasound, and even self-breast exams. Women and men can also assess their risk of breast cancer with genetic screening.
Due to fears of the Coronavirus during the pandemic, many women have delayed their breast screenings. According to the Netherlands Cancer Registry, a quarter fewer cases of cancer have been diagnosed for several weeks. Cancer doesn’t stop for a pandemic so these numbers represent the dramatic drop in women going in for breast cancer screenings. In fact, a poll from the Kaiser Family Foundation shows 48% of Americans say someone in their family delayed or skipped medical care amid the pandemic.
Mammograms are the most common type of breast screening. However, thermography is a safe alternative that evaluates possible areas of concern with no radiation x-rays. When getting a thermography, it is very important to go to a certified thermographer. If a thermography detects any possible areas of concern, the doctor can order a mammogram or ultrasound for further evaluation. Thermography is a method of screening that measures the temperature of the body and produces an image of heat gradation. If there’s an increase in temperature in one area, it may indicate abnormal cellular development and possibly a cancerous tumor. According to the Oxford Academic, radiation is a “universal carcinogen”. So, for concerned patients, it can seem like a double edged sword to get mammogram screenings. This is because they use radiation producing x-ray technology that, according to Johns Hopkins, is equivalent to two months of our normal daily background radiation exposure.
Genetic Screening
Women and men can go one step further by genetically screening for breast cancer. This may be beneficial if an individual has a family history of breast cancer. According to the National Cancer Institute about 5-10% of breast cancer is caused by inherited genes. Having these genes does not mean a definite breast cancer diagnosis will occur in a person’s life. But, if a person does have them, they have up to a 72% risk of being diagnosed with breast cancer and are even higher instances of other cancers according to breastcancer.org.
A genetic counselor can order additional tests for other genes that may also be linked to breast cancer based on a person’s family history. Testing empowers people with knowledge and allows for prevention, early detection, more successful treatments and better outcomes. Every situation is unique. Talk to your doctor or health care provider for more information. Need help with a screening? Visit our Breast Screening Program page here. Click here to visit our free self breast exam pages for men and women to learn what you should be looking for when focusing on early detection.
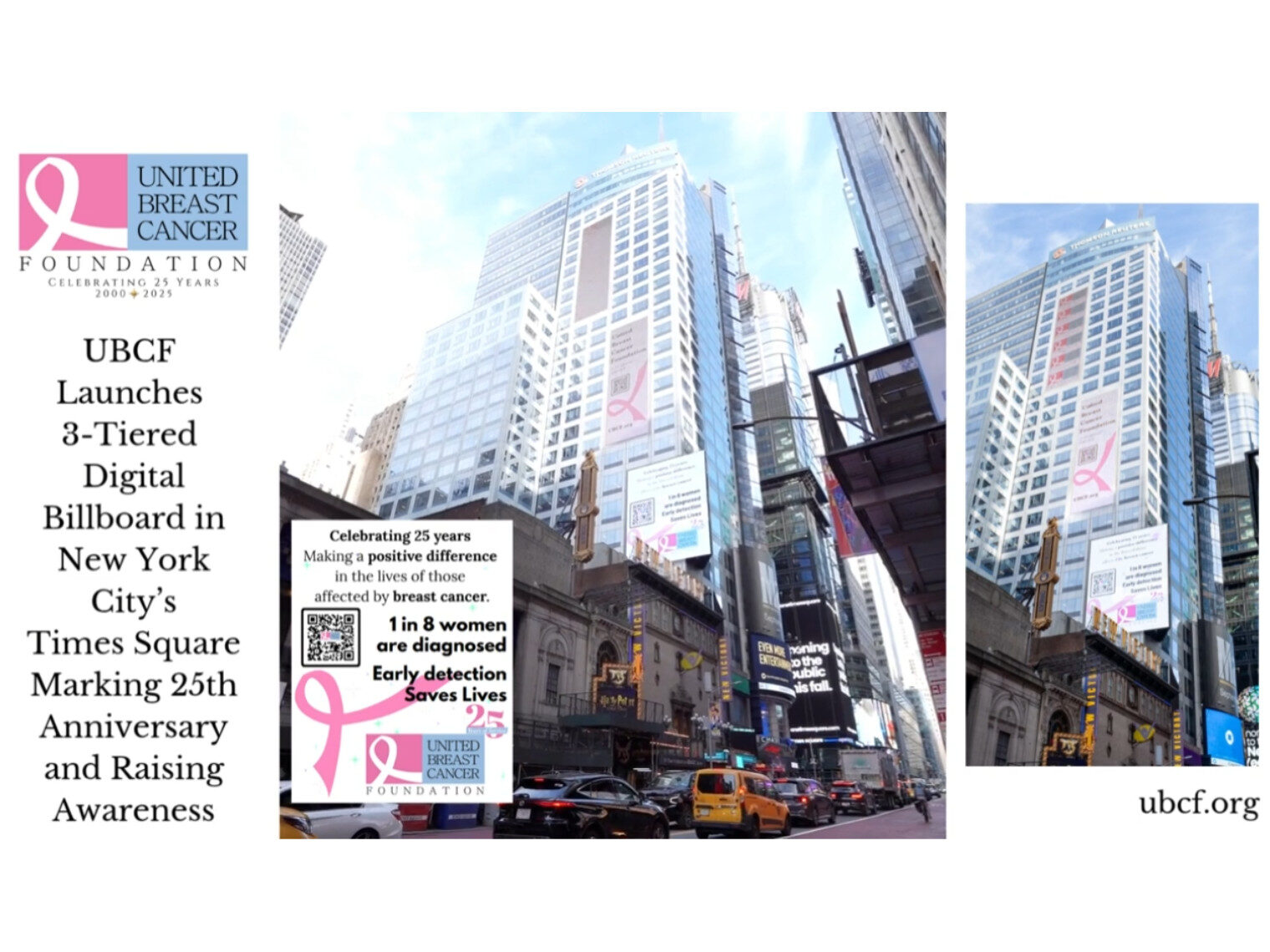
UBCF is here for you! Our Breast Screening Program focuses on providing women and men with free or low-cost breast screenings. UBCF helps to cover thermography, mammograms, ultrasound, and even MRI. If you are interested in finding a low-cost screening location please refer to our website www.ubcf.org, email programs@ubcf.org, or call us at 877-822-4287.